ED physicians, teams sharpen skills, boost confidence with SIM program
Looking back on days when unexpected events forever change lives, the people involved – often those who wind up in emergency rooms – typically say that the day started out like any other. A normal day. Well, today is Thursday. A group of Saint Joseph emergency physicians and providers have gathered for some training when the unexpected happens.
An overhead page. A woman experiencing a high-risk pregnancy has gone into labor in the parking lot.
The group bounds up and heads out. While they never once slow down or break protocol, they are immediately relieved. There is no patient, only a mannequin. This is the training.
One Thursday each month, the Emergency Department Medical Simulation Program, aka SIM, delivers high-quality, targeted, learner-specific simulation experiences to physicians, nurses and EMTs. According to the physician-led leadership team, simulation-based medical education is an essential component of current medical practice, during which real-life clinical scenarios are replicated in an interactive manner, allowing learners to practice rare but critical scenarios in a safe and controlled environment.
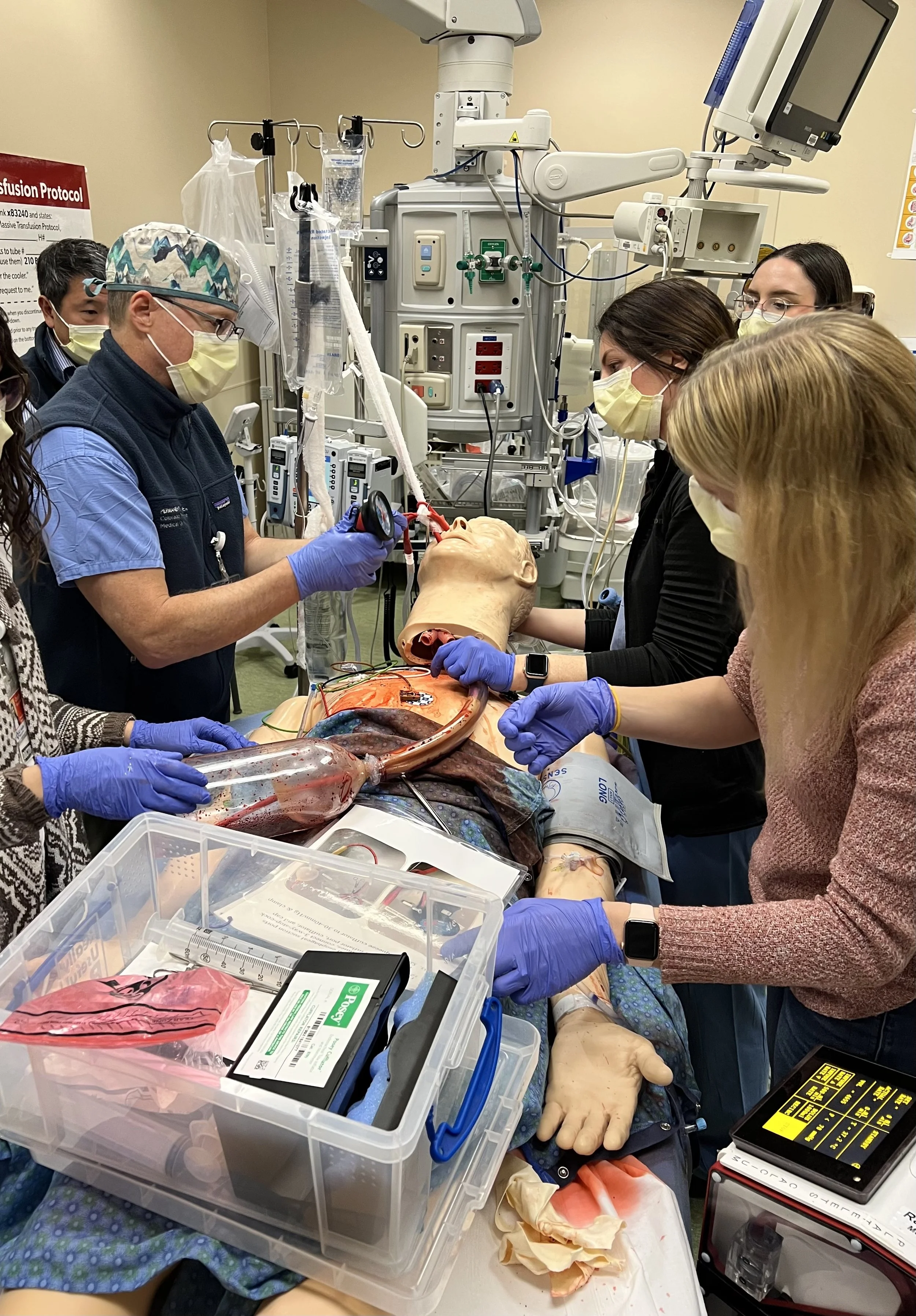
The Saint Joseph SIM Team from left to right: Lisa Maskus, GME simulation coordinator, Goloback, Ekernas, Ed Tham, MD, SIM Program co-medical director, Caitlin Weishar, RN, ED educator. The “patient” shown here needed an emergent cricothyroidotomy and a tourniquet on his leg to stop an arterial bleed that was causing hemodynamic instability. The patient ultimately had to be transferred to a trauma center for definitive care.
Scenarios are unannounced and can include common daily presentations, such as heart attacks and strokes, as well as the uncommon, such as a new mom delivering in the parking lot and a baby who needs neonatal resuscitation.
The SIM: Pre-term delivery in the parking lot. "Mom" showed up in active labor, and the team needed to deliver the neonate outside. Neither breathing nor responsive after delivery, the team had to begin neonatal resuscitation. Mom then had a pre-eclamptic seizure. Reviewed: Delivery protocols outside the hospital, caring for two patients at once, neonatal resuscitation (NRP) and maternal post-delivery complications. Worked in collaboration with NICU and Ob/Gyn educators.
Routine skills are refined and rarely used skills are reintroduced and practiced, ensuring the highest-quality care is provided to every patient who presents on any day. But it’s also much more than that.
“The clinical education provided by SIM, while critically important, is a small part of what makes this training so valuable,” said Molly Goloback, MD, Emergency Medicine and medical co-director of the SIM Program. “Collaboration, teamwork, trust, confidence, communication – these also are skills that need to be practiced, and no exercise challenges and strengthens this skill set as well as a SIM can.”
It’s equally effective at identifying safety risks before any actual patient is impacted. Since its implementation at Saint Joseph in 2014, the ED SIM team has a documented record of identifying and correcting latent safety threats in the ED – such as mislabeled or missing equipment, or misplaced medications – without any risk to patients.
“Inefficient processes, too, can waste critical minutes,” said Karen Ekernas, MD, Emergency Medicine and medical co-director of the SIM Program. “For me, this is the most satisfying and valuable outcome of this program – identifying and correcting systemic issues, troubleshooting and leveling roadblocks to make our protocols run more smoothly.”
Further, this is a site-based SIM program, meaning the scenarios can be developed according to clinical needs unique to Saint Joseph. When the Birthing Center opened across the street, the SIM team developed a mom-baby scenario. When the hospital’s trauma status changed, it developed a trauma scenario.
It’s Thursday. Emergency physicians and team members have gathered for a SIM when a “patient” presents to the ED who is vomiting blood.
The scenario: A massive upper GI bleed. The goals: Recognize the condition, practice a Minnesota tube insertion, initiate the mass-transfusion protocol, activate the Belmont rapid blood infuser. Stay calm.
The SIM: Massive GI bleed. The team had to identify signs of hemorrhagic shock and the cause, initiate the massive transfusion protocol, intubate and place the Minnesota tube. Reviewed: How to place a Minnesota tube. For nurses, the case was a review of equipment location, the mass transfusion protocol and how to run the Belmont.
“I’ve done, maybe, two Minnesota tube insertions in the last 10 years. This is not a common skill, and performing it in front of colleagues in a SIM can be anxiety provoking,” said Goloback. “But that’s exactly why we do it. The SIM is a safe space to remind you, you have the skills you need. This practice will empower you for this patient scenario as well as others.”
“It’s also fun!” said Ekernas. “Our pre- and post-event surveys show SIMs help boost morale and confidence. My advice? Just go for it! You won’t be disappointed.”
ED physicians are required to participate in one SIM every two years, which is just one out of every 24 SIMs. Physicians with questions or those interested in adding a little more extraordinary to an ordinary Thursday can reach out to Goloback or Ekernas for an upcoming SIM schedule.
SIM team works together on upper GI bleed